The ABCD rule (Asymmetry, Border irregular, Colours mixed, Diameter over 6mm) is a useful rule of thumb for evaluating suspicious skin lesions. It is true to say that most melanomas will fail ABCD. However, the rule used alone (without dermoscopy) will miss small, featureless and non-pigmented melanomas, and some of these can be the most dangerous ones. It will also pick up many harmless skin lesions as ‘false positive’ melanomas, and, unless dermoscopy is used to clarify matters, this can lead to needless alarm and unnecessary surgery.
Here is a typical example of a pigmented skin lesion which fails ABCD but is harmless.

Here we see 7 or 8 light to medium brown skin lesions on older white skin. I will add that they are all flat and non-scaly to touch (*). One of the lesions is much larger than all the others and has a very irregular shape. It qualifies as an ‘Ugly Duckling’ and violates the ABCD rule by being Asymmetrical, Border irregular and Diameter well over 6mm (in fact around 15mm diameter). Does this mean we should cut it out? Not without dermoscopy!
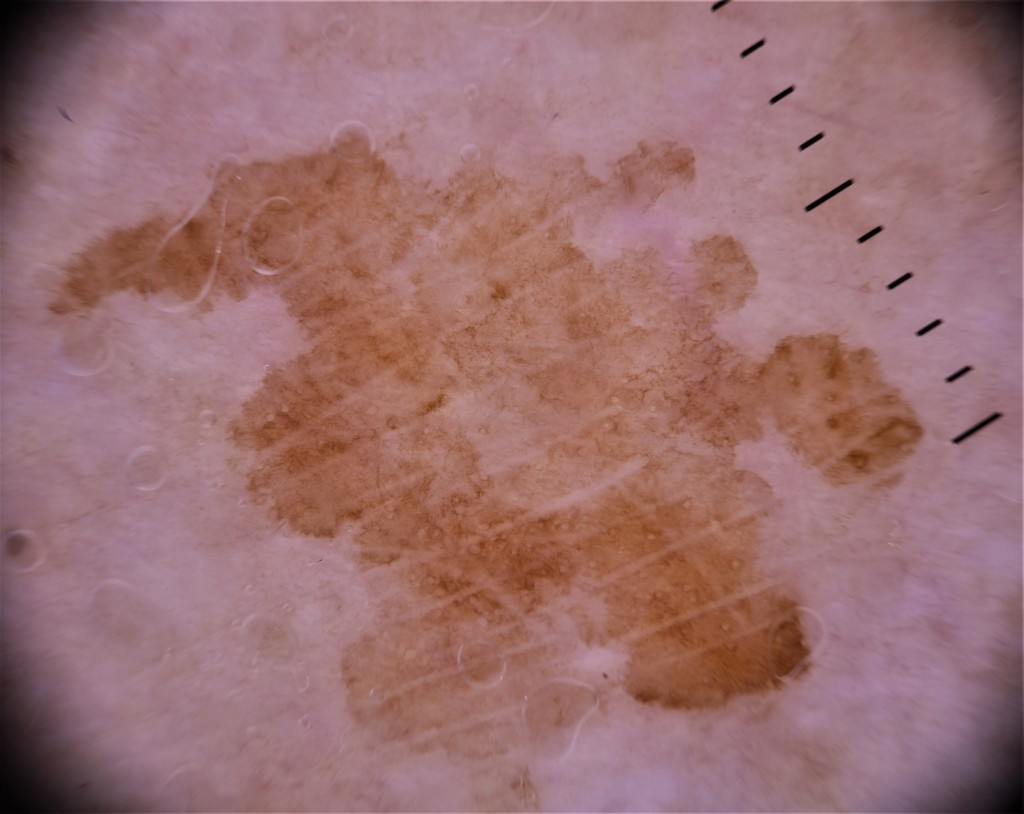
Dermoscopy confirms the very irregular shape. However, experts agree that shape ALONE, although it gets our attention, is not proof of malignancy. The same goes for size. If we get over our initial impression of a very odd shape and study the consistency of the border, we see that although it is very wavy, it is crisp and even in character. You could trace around it easily-the edge is well defined, not wishy-washy and vague. If we have previously used our brain to study the natural history of common skin lesions (*) then we will remember that this even border, even if irregular in outline, is typical of solar lentigo-which is a very common and harmless skin lesion in older white, sun-exposed skin.
The lesions scores A for Asymmetry, B for irregular Border and D for Diameter over 6mm, so that’s 3 out of 4 on the ABCD rule. Colour is OK, I see only brown (mostly light brown, a little medium brown). As far as the dermoscopy is concerned, I call this featureless-there is no overall pattern and it is mostly very homogenous. We can see skin markings, the pale straight lines, and some authorities suggest these may be a weak clue to lentigo maligna, but many others, including me, disagree with that opinion. Certainly there are no other arguable features which are positive for lentigo maligna, which usually have multiple colours, angulated lines, grey or blue areas, inconsistent border, grey circles, granular dots etc.
This lesion was confidently diagnosed as a benign solar lentigo and the patient reassured and advised. I will put up some more examples of solar lentigo (plural lentigines) shortly.
NB the term ‘solar lentigo’ is potentially misleading, given that the word ‘lentigo’ is also used in ‘lentigo maligna’. The use of the word lentigo in both terms may suggest that a benign lentigo can turn into a malignant lentigo. This idea is completely mistaken. A solar lentigo is a pigmented lesion made of pigmented keratinocytes, whereas a lentigo maligna is made up of melanocytes, which are a completely different cell type (by all means click on the links for details). A keratinocyte can no more turn into a melanocyte than a fish can turn into a horse. It is therefore impossible for a solar lentigo to turn into a lentigo maligna. It IS of course possible for fallible humans like us to misdiagnose one for the other! Hopefully studying cases like this will reduce that risk.
NB The term lentigo or lentiginous refers to a particular arrangement of certain skin cells as seen under a microscope. I won’t try to explain what a histopathologist means when he or she says ‘lentiginous’ as it will just confuse matters. Ideally the terms should be changed. If it was up to me I would suggest abolishing the term lentigo maligna and replacing it with melanoma in situ which, as near as makes no difference, means the same thing.
(*) I teach the BEETS holistic diagnostic approach, which stands for
Brain-use your brain to learn all you can about the biology and behaviour of common and important skin lesions
Ears-listen to the patient telling you the story of this skin lesion, how long they have had it, how has it behaved, have they had a skin cancer or high risk occupation etc
Eyes– look at it, and ideally look at the rest of the skin as well for comparison
Touch-light palpation can tell you a lot
Scope-what you have studied skin lesions, listened to the patient, looked at and touched the skin, THEN use the dermoscope. Having done all this, put everything together for your diagnostic hypothesis, and then make a decision whether to reassure, review, refer or remove.
This question is easily answered if you are a dermatologist who earns a fee for every skin check you do. EVERYONE! But in a cash-limited, public funded health care system, we need a certain level of evidence before we roll out a universal screening campaign of any kind. And to date the evidence of benefit for POPULATION skin screening is lacking. However, most experts agree that there is a balance in favour of TARGETTED screening. Good data, the bigger the better, is always welcome as we try to make well informed, safe and just decisions about allocating resources in the face of insatiable demand and limited resources.
A large new meta-analysis (*) in this month’s British Journal of Dermatology ‘Risk factors for subsequent primary melanoma in patients with previous melanoma: a systematic review and meta-analysis‘ by Juliet Smith and colleagues from Sydney, Australia provides such welcome data. The full article is open access so can be freely read and distributed subject to proper citation. It’s findings are hardly Earth-shattering, but such a well-founded study adds a lot of power to those who, like myself, advocate for regular life-long screening for people previously diagnosed with a melanoma and also those without a melanoma diagnosis but who have high risk factors.
What! I hear some readers say. You don’t already have life long screening for those who are known to be at the highest risk of a melanoma? Well, no, not in the British NHS we don’t. Because everything in our government-controlled, cash-limited health system is done according to top-down guidelines from the government agency NICE. They currently say that people with thin melanomas (under 1mm Breslow thickness) should get follow up for one year, thicker melanomas for 5 years (if clinically disease free). Then they are mostly discharged.
Anyway, the BJD paper offers good evidence that if you have had one melanoma, you are at increased risk of a second or subsequent melanoma if you have over 100 moles, even just one atypical mole, red or blond hair, family history of melanoma, a CDK2NA mutation (you would only know this if you had been tested, which isn’t routinely done) older age, evidence of sun damage, inadequate sun protection, first melanoma on head or neck, lentigo maligna subtype, and if you are male. All of these risk factors act independently so the risk adds up. The authors say that studies have shown the increased risk can range from 10 fold to 25 fold. That’s a lot. I have seen an Italian study where people with a melanoma had an 8% risk of getting another new one in the next 5 years.
It was my opinion for some years before I retired from clinical practice last year (since retiring I am free to speak my mind fearlessly) that anyone who had been diagnosed with a melanoma and also had over 50 moles should certainly get education, total body photography and life long surveillance, but the underfunded and badly organised British National Health Service did not provide for this. The publication of this very good piece of research supports my opinion, but it will most likely be ignored unless a sufficient amount of public opinion builds up. In the meantime, I continue to encourage GPs and other interested health care professionals to see a business opportunity to upskill in skin lesion diagnostics and offer affordable private skin checks.
Here is a case in point. A very thin melanoma picked up on a routine skin check.

It’s small, but it’s a funny shape, different to the other moles (ugly duckling) and IT WASNT THERE AT THE LAST SKIN CHECK.
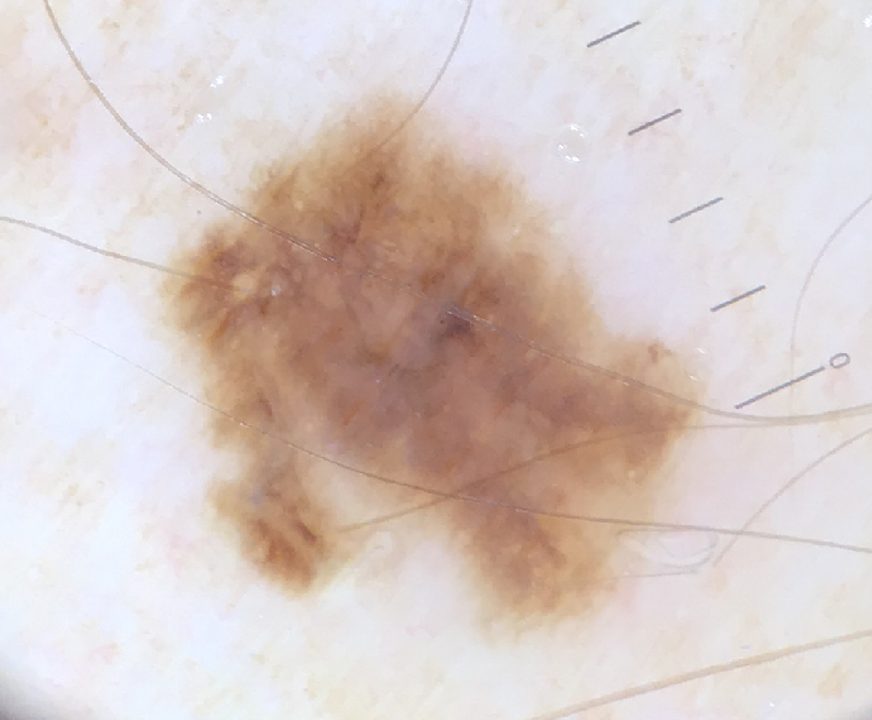
The dermoscopy is essentially featureless, there is no overall pattern. You could argue for some irregular clods or faint angular lines, but I can’t see any really positive melanoma clues. HOWEVER we don’t just rely on dermoscopy, but on integrated lesion diagnostics, which takes into account that the patient is older, white, sun damaged, previously had a melanoma and this is a new lesion on sun exposed skin, and to the naked eye it looks a funny shape. Add to that, dermoscopy does not positively confirm one of the 5 common benign skin lesion types (naevus, keratosis, haemangioma. dermatofibroma, sebaceous gland hyperplasia) so by default we have to rule out melanoma.
This was an in situ melanoma, the earliest grade and 100% curable. We cannot say for certain that if this super-thin melanoma had not been picked up by a skin check that it would have gone on to metastasise, but we know that this is possible. Managing one patient with stage 4 metastatic melanoma can consume £500,000 or more of immunotherapy and other costly modern oncology drugs, and the patient may still die. When we have solid evidence that patients with a primary melanoma diagnosis have a significant increased risk of getting another new melanoma, and they get life long follow up in most countries, but not in Britain, something doesn’t seem right. It seems as if the establishment is more willing to pay £billions for oncology at stage 4 than £millions for earlier detection at stage 0 or 1.
Of further comment, it is recognised by experts in skin screening like Scott Menzies and Harald Kittler, that very early melanomas are often featureless, and as such will ONLY be picked up by digital screening, whereby there are photos of the skin that can be used for comparison. They develop features as they get thicker-and deadlier.
It is an interesting thing that most Britons don’t trust their politicians, but want them to be in charge of health policy and delivery.
(*) A meta-analysis, for those not in the know, is a ‘study of studies‘ produced by a team of workers, who may be statisticians rather than medically qualified, who search all known databases, pull out all the relevant research of sufficient quality, and use statistical methods to ‘average out;’ the findings. This has the effect of producing a piece of research which is much bigger, and therefore more valid, than the individual trials that went into it. A good meta-analysis that is good enough to get into a prestigious peer-reviewed journal will have been rigorously tested and is the nearest think to absolutely positive proof we are going to get.
Every now and then, we hear of a famous person being diagnosed with skin cancer and lots of articles appear, not always very well informed. It specially gets up my nose that while articles often include descriptions of what to look out for, for example lesions that bleed, break the ABCD rule, etc, we seldom see many useful pictures of melanomas. There are plenty in the public realm, for example on this blog. I’d let them have some images for free if they asked nicely.
The most recent celebrity melanoma patient is Sarah ‘Fergie’ Ferguson, Duchess of York and ex-wife of Prince Andrew (*). I hope she will be among the 90% of melanoma patients who are cured through early enough diagnosis: I have no ghoulish interest, but it is legitimate to comment on what is in the public realm.

Popular British newspapers have posted extensive discussions about Sarah Ferguson’s melanoma recently, such as here in The Daily Mail and again in The Sun. In both articles, there are multiple colour photos of the lady in question and other members of the Royal Family, but no pictures of melanomas! What a wasted opportunity!
I have read several on line pieces about the Duchess of York’s melanoma diagnosis, and didn’t think much of the informational content of any of them. It will be interesting to see if the publicity leads to more people seeking advice about funny looking moles. Anyway, I was sorting out some old BJDs a few days back and came across this article from last April about false beliefs and misguided advocacy around sun protection for skin cancer prevention (see link) which I thought was a good bit of writing not just about sun protection but misinformation in general.
False information (fake news) is swallowed because, according to the article, we tend to trust sources that appear ‘attractive, powerful and similar to ourselves.‘ It is surely better to try to find sources which are evidence based and balanced, since many journalists just copy from other journalists, who may not be so well informed as they would like us to think. And the issues sometimes can’t be simplified beyond a certain point.
There has been a lot in the news lately about the British Royal Family’s health issues. Since King Charles has had some prostate trouble recently, enquiries to the National Health Service web page about prostate disease has increased greatly. It is possible that the Duchess of York’s melanoma diagnosis may drive further interest in getting skin checks. But the NHS does not routinely offer skin checks, and indeed British GPs are seldom trained enough to do them very well. Which is a good time to mention the Skin Cancer Symposium’s excellent 2 day skin lesion diagnostics conference in Manchester this summer. Early bird price is pretty good value at just £700 which will include a free copy of Cliff Rosendahl’s excellent book which he will be there to sign.

(*) Prince Andrew is currently disgraced and not performing royal duties following accusations of sexual impropriety around the Jeffrey Epstein revelations. I have no more to say here about that or other British Royalty issues.
A position statement appeared in a recent Journal of the European Academy of Dermatology and Venereology (JEADV) was recently published. It was a thoughtful and thorough piece of work by the EADV Task Force on Artificial Intelligence (AI), led by various luminaries of the skin cancer diagnostics world including Professor Harald Kittler, whom regular readers here will know is held in admiration for his brilliant mind, body of work and devotion to skin cancer diagnostics research. It is an open access article which can be freely read and downloaded.
Read it yourself if you are interested, but in summary the statement says that Artificial Intelligence in dermatology, including Smartphone apps, is already here and has great potential for good, but could also do some harm if we’re not careful, so we ought to keep an eye on it to make sure it is done right and not used to frighten and exploit people.
I thought of this as I came across the following case from my image archive, which I am currently editing and setting in order since I have now retired from clinical practice and wish to pass on when I pass on. This case was of a young-ish person with a long standing mole on a limb. They took a picture of it and fed it into a mobile phone application, which said it was worrying and told them to seek advice. They went to their GP, who unsurprisingly made an urgent skin cancer referral, although there was no history of recent change or other pointers to a skin cancer.
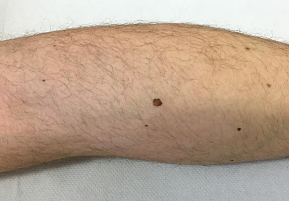
This is a mole of slightly above average size on a white adult, larger than the other 5 or 6 moles in view, but not dramatically so. Importantly, it had been there for years and there was no recent change. So far, I am not very anxious, but let’s take a closer look.

It’s not a great photo, but doesn’t raise any red flags. Let’s get the dermoscope out.
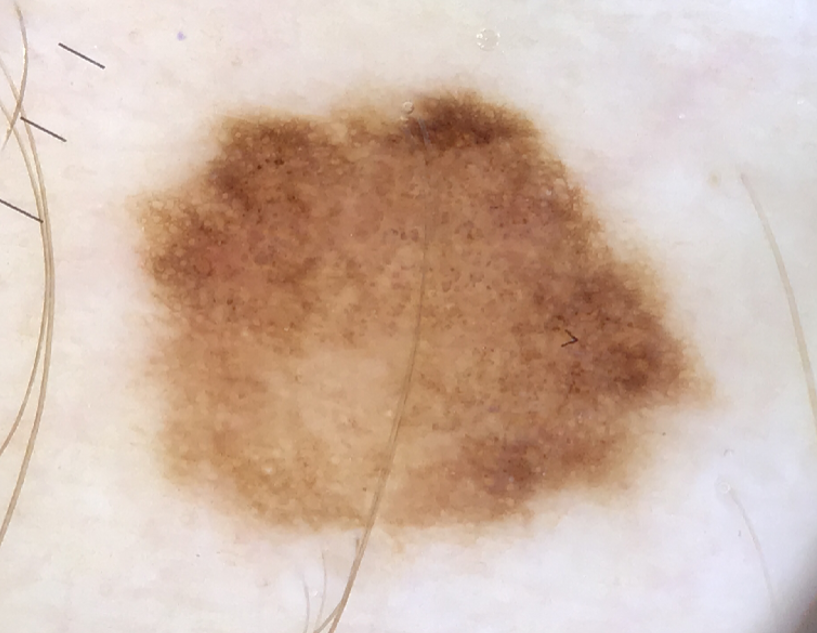
This is really a very bland mole. It is essentially featureless, with fairly good symmetry (the slightly darker area at the top too trivial to count), a little reticular network around the periphery from 10 to 3 o’clock, fairly even border and no positive melanoma clues. My judgment was that this was a bland naevus with no worrying features and could be safely observed.
However, by this time the patient was frightened. They had been initially scared by the AI Smartphone app, then by their GP’s failure to reassure (not surprising since British GPs get about half an hour of skin lesion recognition training in a lifetime, they all live in fear of being sued or complained against, and they have nothing to lose by referring all such cases to hospital) and of course they had been summoned urgently to the SKIN CANCER clinic with a letter that had the word CANCER all over it. They were not prepared to accept my reassurance.
The lesion was duly cut out and examined by two of our expert histopathologists, who duly confirmed my informed and experienced judgment that this was an entirely harmless naevus, not even ‘mildly dysplastic.’
SO, a lot of fuss and trouble, and a permanent scar, because of a for-profit Smartphone app which had never been signed off by any medical authority and will UNDOUBTEDLY have been set at an extremely high sensitivity/low specificity diagnostic level in order to make sure the app’s makers will never, ever be sued for a missed melanoma. ‘Better safe than sorry’ as the saying goes? They won’t be the ones dealing with the needless anxiety and extra work generated by their profitable product.
OK, that’s one story. But it’s not the only one I have come across, and Alan Halpern, a leading New York skin cancer professor, said at the EADV in Milan in September 2023 that they were already seeing big problems in America and Scandinavia due to overdiagnosis by these AI devices. The professor said ‘These Smartphone skin lesion diagnostics apps are going to send us a huge amount of extra work.’ In a health care system where more work means more item of service fees and increased profits, they will not be weeping much over this. But it’s a different matter in a cash-limited service like the British NHS where we have rationing by queue. If more people join the queue, it gets longer.
I agree with the EADV Task Force that there are benefits to be had from AI dermatology Smartphone apps. But as with everything else that clever (but not always wise) humans come up with, there will be a down side as well. Let’s be careful out there. As I write in January 2024, Britain is reeling from the Post Office false accounting scandal, which was caused by a bad piece of software and by managers promoted above their level of competence who refused to entertain the possibility that the software could be wrong. It was wrong, badly, and many lives were ruined.
I an glad to announce that there will be a World Day of Dermoscopy run by the International Dermoscopy Society in partnership with various other non-invasive world skin diagnostics bodies on Saturday 11th May. Top world speakers will address a wide range of subjects, and thanks to our sponsors it will be free of charge to health practitioners who register. Details Here.
I am honoured to have been asked to give a presentation on the dermoscopy on non-pigmented benign skin lesions. The scientific committee is led by such luminaries as Professor Giuseppe Argenziano of Italy and Professor Aimilios Lallas of Greece, Professor Awatef Kelati of Morocco is scientific organiser, and speakers of the highest quality from around the world will be teaching.
The full programme isn’t published yet, but the abstract below gives an idea. As you can see, it will not just be about the diagnostics of benign and malignant lesion but also the application of dermoscopy to other cutaneous problems including issues around varying appearances in skin of diverse colours.
I recommend early booking, the last time the IDS put on a free global meeting like this (to replace the planned regional conference in Warsaw, Poland in 2020 that was cancelled by Covid) it was our most popular meeting ever with 6,000 delegates leading to strain on the broadcasting technology!
